Use OASIS Guidance to select the best answer.
1) Your agency received a new referral for a patient with Medicare and a physician’s order for PT three times a week for 4 weeks and nursing for 1 visit to remove staples in 5 days.
Which approach is compliant?
a. The PT may do the initial assessment visit, but the RN must do the SOC comprehensive assessment.
b. The RN must do the initial assessment visit, but PT may do the SOC comprehensive assessment.
c. The PT must do the initial assessment visit and the SOC comprehensive assessment.
d. The RN must do the initial assessment visit and the SOC comprehensive assessment.
2) Your patient has a past cardiac medical history and is sent to the ED with chest pain. From the ED he is transferred to the cardiac floor for observation where he remained for 3 days until being admitted to an inpatient bed. He was discharged home after 20 hours as an inpatient. Your Intake department verified the observation and inpatient status timing with the hospital billing department when accepting the referral.
Which of the following represents appropriate OASIS data collection?
a. Only the RFA 6 Transfer to Inpatient Facility – Patient not discharged is appropriate
b. Both RFA 6 Transfer to Inpatient Facility – Patient not discharged and RFA 3 ROC are required
c. Either the RFA 6 Transfer to Inpatient Facility – Patient not discharged or the RFA 7 Transfer to Inpatient – Patient discharged could be completed
d. No OASIS is required
3) Mr. Tom’s SOC was on January 14 by the PT. Orders also included OT and home health aide services. The PT called to schedule the agency discharge visit for Jan. 25. Mr. Tom refused the visit stating he was going to begin Outpatient PT that day. Mr. Tom was discharged on Jan. 24 per agency policy. The PTA was the last to visit Mr. Tom on 1/22. Agency policy allows for a collaborative assessment process.
Visits received during the HH episode:
• PT Jan. 14
• PTA Jan. 16, 18, 20 and 22
• OT Jan. 17, 19
• Aide Jan. 15, 17 and 19
What is the most compliant way to complete the discharge OASIS assessment?
a. The PT must complete the discharge assessment based on Mr. Tom’s status on his/her last visit of Jan. 14.
b. The PT may complete the discharge assessment based only on visits made in the last five days of care; in this scenario, the PTA and aide visits made on or between Jan. 20-24.
c. The OT may complete the discharge assessment based on his/her visit of Jan. 19 supplementing it with information from the last five visits made to the patient.
d. The OT may complete the discharge assessment based on his/her visit of Jan. 19 supplementing it with information from the PTA and aide visits made on or between Jan. 18-22.
4) Which of these statements about pressure ulcers/injuries is TRUE?
a. The unstageable response/code for a pressure ulcer/injury initially observed and documented in the pressure ulcer/injury items as being covered with a non-removable dressing at the SOC should be corrected when the dressing is removed, and the ulcer/injury is observed later in the assessment time frame.
b. A pressure ulcer treated with a skin graft is a surgical wound.
c. A stage 3 pressure ulcer completely covered with new epithelial tissue is reported as a Stage 3 pressure ulcer in OASIS.
d. A previously stageable Stage 4 pressure ulcer that is now covered with eschar is reported as a Stage 4 pressure ulcer.
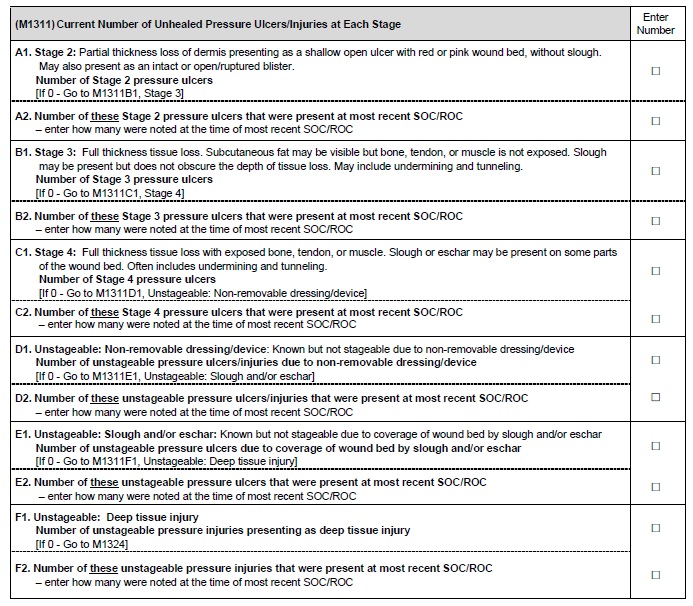
5) At the discharge visit, Mrs. Richardson has two pressure ulcers:
1. Right hip – a Stage 3 that was a Stage 2 at SOC
2. Right elbow – a Stage 4 which is fully granulated
Your record review shows that at SOC, the ulcer/injury on the right elbow was unstageable due to a non- removable dressing. Three days after the SOC, the dressing was changed and the ulcer was observed to have 50% slough with a tendon visible.
How do you complete M1311 at Discharge?
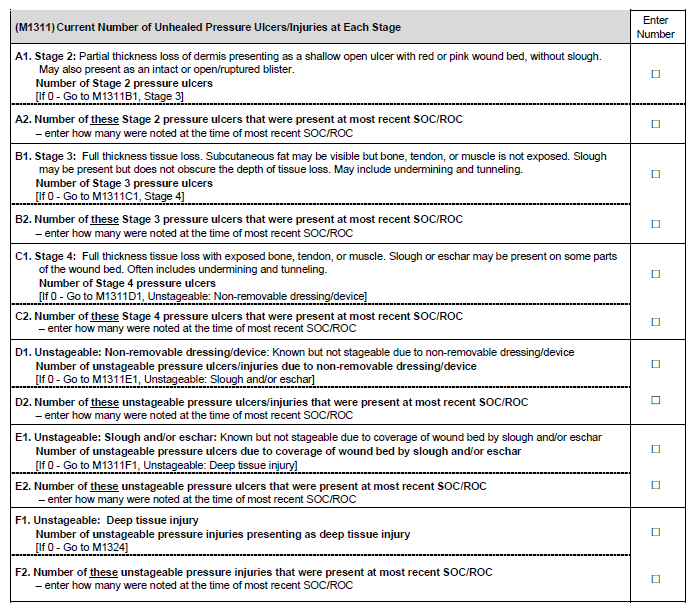
6) Mrs. Torres is assessed to have pressure ulcers in three locations:
1. Left elbow – a Stage 3 at DC; was a Stage 1 at SOC
2. Left ischium – a Stage 4 at DC; was 100% covered with eschar at SOC, then debrided and assessed as a Stage 3 one week after SOC
3. Sacrum – covered with eschar at DC; was a Stage 2 at SOC
How do you complete M1311 at Discharge?
7) Mr. Adams had a cholecystectomy performed via laparoscopic surgery 10 days ago and you are admitting him to home care following exacerbation of his CHF post-op. His 1 cm incision was closed with a chemical bonding agent and is assessed to be completely closed, clean and dry with no signs of infection. Additionally, Mr. Adams has an implanted Baclofen infusion pump and the puncture site where the reservoir was filled in the hospital is reddened and tender.
How do you complete M1342 Status of Most Problematic Surgical Wound that is Observable?
a. 0 – Newly epithelialized
b. 1 – Fully granulating
c. 2 – Early/partial granulation
d. 3 – Not healing
8) Which statement regarding M1021 Primary Diagnosis and M1023 Other Diagnoses is TRUE?
a. A diagnosis represented by a Z-code is permitted as a primary diagnosis.
b. The coder who has not seen the patient may determine the primary and other diagnoses and symptom control rating.
c. M1023 Other Diagnoses may be listed in any order.
d. The diagnoses listed in M1021 and M1023 must always be actively addressed in the patient’s Plan of Care.
9) Mrs. Stevens was referred for home care because she is experiencing severe symptoms related to an outbreak of shingles on her right lower abdomen. Her past health history is negative for any chronic illness.
How do you complete M1028 Active Diagnoses at the SOC?
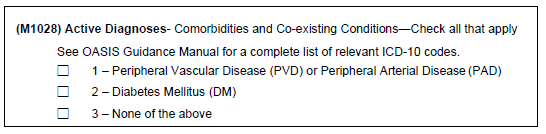
a. Leave all boxes blank/empty.
b. Select box 1 and box 2 and box 3
c. Select box 3 only.
d. Enter a dash “(-)” in box 1 and box 2 and box 3
10) During your SOC assessment interview, Mrs. Hatfield reports that she had never been in the hospital until she fell off a curb 5 months ago and broke her ankle. She was taken to the ER and then hospitalized for surgical repair of her ankle and several days of antibiotics. In the last month, she has noticed that she can’t do what she used to every day. She tires easily and recently started napping in her chair while watching her game shows in the afternoon. Her doctor is running tests. She takes a vitamin, a laxative and an occasional over the counter pain reliever for headaches.
How do you complete M1033 at the SOC?
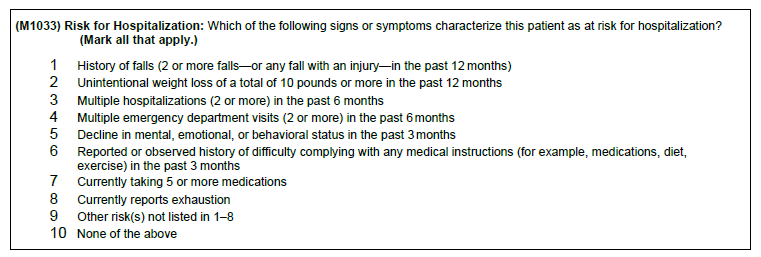
a. Select 1 and 8 only
b. Select 3 and 4 only
c. Select 1, 3, and 4 only
d. Select 3, 4, and 8 only
11) Mr. Howell was admitted to your agency on February 1, and his SOC weight/height was measured and documented as 154 lbs. and 5 feet 7 inches. He was transferred to the hospital on February 10th with severe back pain. At the ROC visit on February 14, Mr. Howell could not be weighed accurately due to the presence of his back brace which was not to be removed. His height was measured following agency policy as 5 feet 7 inches.
How do you complete M1060 Height and Weight at ROC?
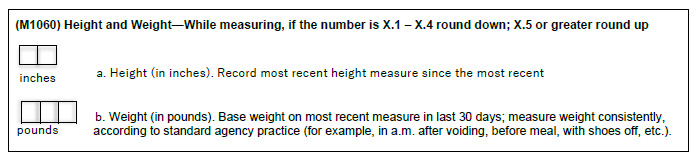
a. Height – 67 inches; Weight – enter a dash “(-)”
b. Height – 67 inches; Weight – leave the box empty/blank
c. Height – 67 inches; Weight – 154 lbs.
d. Leave both boxes blank
12) Mrs. Roberts lives with her son who is paid to take care of her under a State funded program. John is available in the home to provide care every day and night of the week except Saturday. Each Saturday, he volunteers at the local Food Bank from 8 AM until 4:30 PM. During that time, he keeps his cell phone handy, so his mom can call him if there are any emergencies.
What is the correct code for M1100 Patient Living Situation?
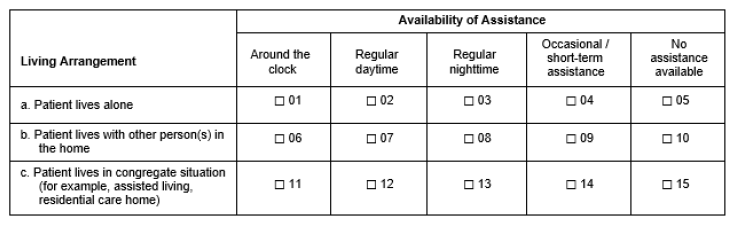
a. Code 01
b. Code 03
c. Code 08
d. Code 09
13) At SOC, you determine that Mr. Brooks requires assistance at all times to ambulate safely even though he lives alone. He ambulates with your supervision to the bathroom and is able to perform his grooming independently and safely by standing at the sink and sitting on the toilet as needed.
Select the correct code for M1800 Grooming.
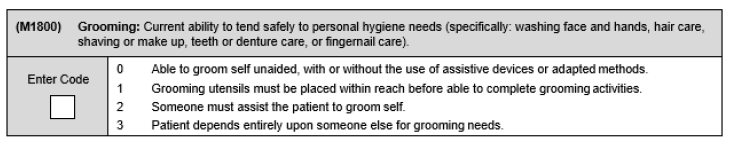
a.Code 0
b. Code 1
c. Code 2
d. Code 3
14) Mrs. Baker lives with her daughter. The home is being remodeled to accommodate the patient’s needs. At the time of the SOC comprehensive assessment on Tuesday, the only bathroom is under construction and not available, therefore Mrs. Baker is using the kitchen sink to wash up. She is able to wash everything without her daughter’s help except her hair.
What is the correct code for M1830 Bathing?
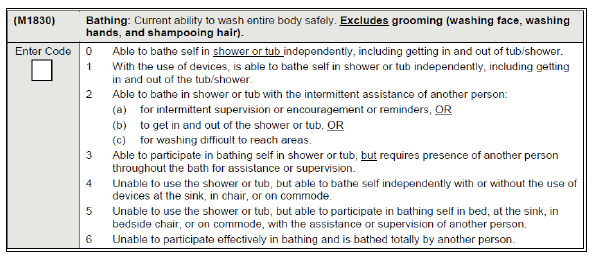
a. Code 2
b. Code 3
c. Code 4
d. Code 5
15) Mr. K has difficulty seeing on his left side since his stroke. At the time of discharge from your agency, his son still needs to remind him during the meal to scan the entire plate to ensure he has seen all the food.
What is the appropriate code for GG0130 Eating at Discharge?
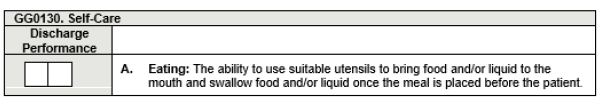
a. Code 06, Independent
b. Code 05, Setup or Clean-up Assistance
c. Code 04, Supervision or Touching Assistance
d. Code 03, Partial/Moderate Assistance
16) Mr. Gold is feeling weak and dizzy. After a struggle, he is able to get himself closer to the edge of the bed but is unable to get himself up and to a seated position. His wife helps lift his upper body up from the bed and you provide additional assistance and cues necessary for the safety of the patient and his spouse. With some therapy and a hospital bed, you think that Mr. Gold will be able to get from lying to sitting with only verbal cueing at discharge.
How do you code GG0170C1 SOC/ROC Performance and GG0170C2 Discharge Goal?
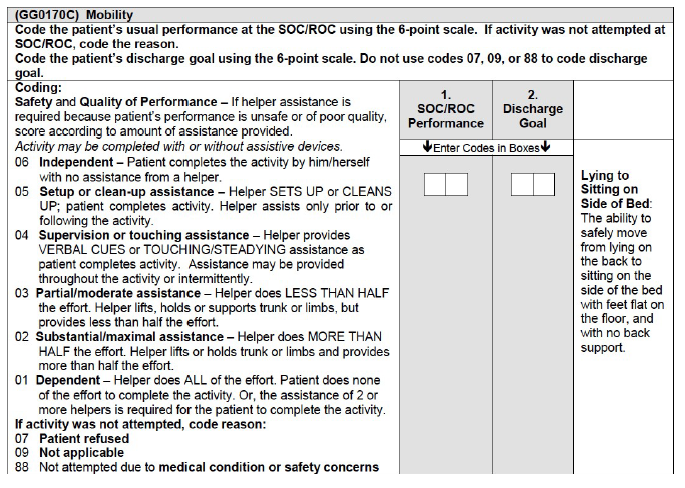
a. SOC/ROC Performance 04 Discharge Goal 05
b. SOC/ROC Performance 03 Discharge Goal 04
c. SOC/ROC Performance 02 Discharge Goal 04
d. SOC/ROC Performance 01 Discharge Goal 04
17) When asking the patient about falls on the discharge visit, Mr. E and his spouse report that one day he had a “near miss” when the therapist was teaching him to use his walker and he stumbled. The therapist “caught him” and prevented Mr. E from falling to the ground avoiding any injury. There was no other evidence of a fall when reviewing the medical record.
Select the correct codes for J1800 Any Falls Since the SOC/ROC and J1900 Number of Falls Since the SOC/ROC?
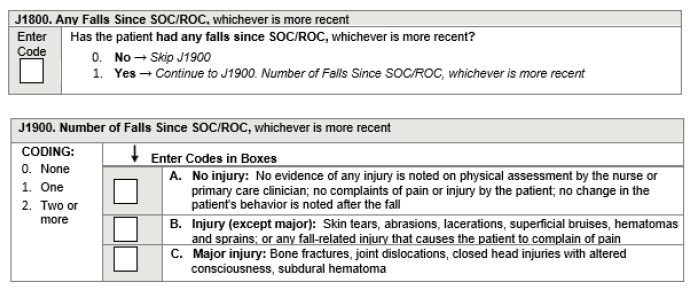
a. J1800 – 0; J1900 skipped
b. J1800 – 0; J1900 A. (1), B. (0), C. (0)
c. J1800 – 1; J1900 A. (0), B. (0), C. (0)
d. J1800 – 1; J1900 A. (1), B. (0), C. (0)
18) You admitted Mr. Jones to home care with 11 prescribed medications. As you performed the drug regimen review, you discovered that he only had 10 of the meds in the home. When questioned, he stated the other medication was an over-the-counter med, was not covered by his insurance, and he couldn’t afford it. You believed the med was critical to his care and called the physician on the SOC visit. The physician called in a prescribed alternative the same day which the insurance covered and you arranged for his daughter to pick up the medication from the pharmacy during her lunch break. You reported the clinically significant medication issue in M2001 Drug Regimen Review and selected Yes for M2003 Medication Follow-up. Mr. Jones was not hospitalized during the episode of care and no additional medication issues were identified before his discharge from the agency.
At Discharge, how do you code M2005 Medication Intervention?

a. Item would be skipped
b. 0 – No
c. 1 – Yes
d. 9 – NA
19) Mr. Murphy, who is legally blind, has been taking 3 once-daily medications p.o. each morning. Recently, he was ordered to take a benzodiazepine wafer at bedtime sublingually. On the day of the assessment, he stated he had no problem taking his regular once-daily medications as long as his nephew comes over on Sunday and fills his medi-planner for him. Examination of the medi-planner supported this report. Mr. Murphy confessed he hadn’t started his new medication for his panic attacks because he didn’t understand what the doctor meant by the word “sublingual.”
What is the correct code for M2020 Management of Oral Medications?
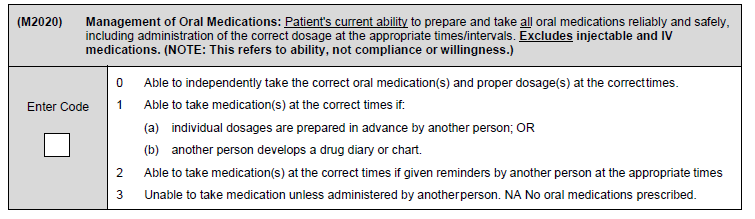
a. Code 0
b. Code 1
c. Code 2
d. Code 3
20) Mrs. Cook lives alone but has 2 daughters who are very active in her care. At the time of the discharge, one daughter stops over each morning to help her mom shower. Mrs. Cook sometimes forgets to make her dinner and take her evening medications and the 2nd daughter stops by each evening to help her with these activities. Mrs. Cook has no medical treatments ordered.
How do you code M2102 Types and Sources of Assistance rows a, d and f at discharge?

a. Row a – 1; Row d – 0; Row f – 1
b. Row a – 0; Row d – 0; Row f – 0
c. Row a – 1; Row d – 0; Row f – 0
d. Row a – 0; Row d – 1; Row f – 0