COS-C Exam Preparation
Exam Description
- 2.5 hour “open book” examination
- 100 multiple choice questions
- At Exam Check-in time, candidates must present 2 forms of Identification, one of which must be a valid government-issued ID.
- Content based on the current OASIS data collection rules and guidance provided by CMS (Visit our Resources page).
- Exam results are reported as Pass or Fail.
- Exam score is based upon the number of questions answered correctly.
- COS-C exam pass rate for 2024 was 77%, that is, 77 out of every 100 candidates achieved a passing score in 2024.
General Guidance
- Arrive at least 30 minutes prior the exam time to sign-in and get settled.
- Candidates must be signed in and seated 15 minutes before exam start time or tardiness may cause candidate to forfeit some of the 2.5 hour exam time.
- Exam is open book & open notes: Candidates are allowed to bring ANY paper-based OASIS reference materials into the examination, including, but not limited to CMS core OASIS Documents, OASIS Guidance Manual, CMS OASIS Q&A’s, the Blueprint for OASIS Accuracy handout and an INSTANT OASIS Answers book. Reference materials may include handwritten notes, loose notes, tabs and flags as page markers.
- Electronic equipment of any kind may not be used in or out of the exam room during the testing time. Cell phones will be turned off.
- At Pencil & Paper test, beverages are permitted in the testing environment at your own risk. No additional time is given to clean up a spill. At Computer-Based Tests (CBT), NO beverages are allowed in the testing room.
- Food is not allowed in the exam room except for medical reasons.
Independent study of the current OASIS data collection rules and guidance provided by CMS is encouraged though is not required. - Successful candidates will understand the intent of each OASIS item and have a working familiarity with all the special rules included in the Response-Specific Instructions and Coding Tips for each item in Chapter 3 of the OASIS Guidance Manual and with related CMS Q&As. Candidates may be presented with a question that is testing knowledge of a fact regarding an OASIS item. Alternatively, candidates may be presented with a scenario, and asked to determine which response option should be selected for a particular OASIS item, based on the details provided in the Exam scenario. The Exam scenario will provide all the details needed to successfully apply the CMS guidance and select the single correct response. The Exam is open book, so as time allows, candidates will be able to consult their references as needed.
- Use the domain descriptions below as a guide for any exam review and preparation and try the sample questions that are included.
Description of COS-C Exam Domains with Sample Questions and Study Resources
- Time Points & Patient Populations
- Administrative & Patient Tracking
- Regulations
- Diagnoses & Sensory
- Bowel/Bladder, Nutrition & Wounds
- Cognition & Mood
- ADLs/IADLs
- Medications & Special Treatments
- ED Use, Inpatient Transfer & Discharge
- Functional Abilities
Description: This Domain tests your knowledge of situations and events which trigger mandatory OASIS data collection as well as knowledge regarding which patients require OASIS data collection. You will need to understand when OASIS data for Start of Care, Resumption of Care, Recertification, Other Follow-up, Transfer, Death at Home and Discharge is required to be collected. A good understanding of Time Points means that you not only can identify specific situations when OASIS data must be collected but can also discern when OASIS data collection would not be required. You could be presented with scenarios that include information such as the patient’s age, payer, discharging facility, services ordered, events occurring during or following the clinician’s visit and be required to apply the CMS guidance to determine if OASIS data collection would be required.
Sample Questions for this Domain:
Question: On a routine revisit, your patient tells you that since the last time you visited she has had a three-day in-patient hospital stay to treat an exacerbation of COPD and now has several new medications which she doesn’t know how to take properly. Select the response that reflects the OASIS data collection required by the scenario described.
a. No OASIS data collection is required
b. RFA 5 Other Follow-up assessment
c. RFA 6 Transfer to an inpatient facility-patient not discharged from agency, and RFA 3 Resumption of Care assessments
d. RFA 4 Recertification assessments
Correct Response: (c)
Question: Which of the following patients requires OASIS data collection?
a. A 78-year-old patient with a primary diagnosis of Heart Failure admitted to the Hospice Medicare benefit.
b. A 17-year-old victim of a gunshot who requires daily packing of a wound; Medicaid is the payer.
c. A 47-year-old patient who qualifies for Medicare disability insurance and requires diabetic teaching and drug monitoring.
d. A 31-year-old patient with a wound infection that is status-post Cesarean section.
Correct Response: (c)
Description: This Domain tests your knowledge of the CMS OASIS guidance related to coding items collecting information on patient characteristics and demographics.
Sample Question for this Domain:
Question: During the SOC comprehensive assessment for home care admission following a recent CVA, your patient expresses that his biggest concerns are his difficulty with speech and his inability to drive a car. He has always been independent in driving himself wherever he needed to go. When you ask about getting to medical appointments or errands, the patient has some difficulty being understood with his speech but is able to communicate that transportation will not be a problem, as his son and daughter-in-law live behind him and have agreed to make sure he gets to his appointments and errands. Which of the following is the correct response for A1250 – Transportation?
a. B. Yes, it has kept me from non-medical meetings, appointments, work or from getting things that I need
b. C. No
c. X. Patient unable to respond
d. Y. Patient declines to respond
Correct response: (b)
Description: This Domain tests your knowledge of the OASIS CMS Regulations regarding OASIS data collection. Specifically, you will need to have a good working knowledge of the Condition of Participation, Section 484.55, The Comprehensive Assessment of Patients; including each of the Condition Standards: Initial assessment visit, Comprehensive assessment, Drug regimen review, Update of the comprehensive assessment and Incorporation of OASIS data items.
Sample Question for this Domain:
Question: The Conditions of Participation require that a drug regimen review be performed as part of:
a. Every comprehensive assessment
b. The Start of Care comprehensive assessment only
c. The Start of Care, Resumption of Care and Discharge comprehensive assessments only
d. The Start of Care, Resumption of Care, Recertification, and Discharge assessments only
Correct Response: (a)
Description: The Diagnoses and Sensory Domain tests your mastery of OASIS item-specific guidance and scoring conventions for items collecting data on the patient’s sensory status, including hearing, vision, pain, and items related to reporting of patient diagnoses.
Sample Question for this Domain:
Question: You are completing your patient’s SOC assessment with her daughter present. As you move into the living room to complete a portion of the assessment, the patient asks her daughter to turn down the television so she can better hear your instructions. The patient confirms that hearing conversations is little more difficult, and she tries to minimize unnecessary noises so she can better participate in family discussions. What is the correct response for B0200. Hearing?
a. 0. Adequate- no difficulty in normal conversation, social interaction, listening to TV
b. 1. Minimal difficulty-difficulty in some environments (e.g., when person speaks softly, or setting is noisy)
c. 2. Moderate difficulty- speaker has to increase volume and speak distinctly
d. Highly impaired – absence of useful hearing
Correct response: (b)
Description: This Domain tests your mastery of OASIS item-specific guidance and scoring conventions for items collecting data on patient nutrition, incontinence, UTIs, pressure ulcers, stasis ulcers and surgical wounds.
Sample Questions for this Domain:
Question: At the Start of Care, your patient has a Stage 1 pressure ulcer on his right elbow, a Stage 2 pressure ulcer on his left elbow and a Stage 4 pressure ulcer on his left hip that closed 4 years ago.
Select the answer that contains the best responses for M1311 at the SOC assessment:
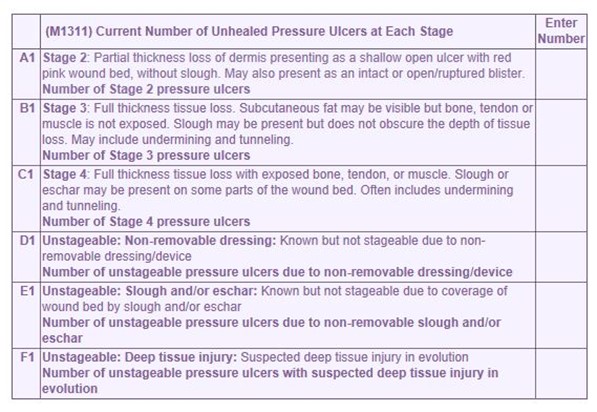
a. A1 = 1, B1 = 0, C1 = 0, D1 = 0, E1 = 0, F1 = 0
b. A1 = 1, B1 = 0, C1 = 1, D1 = 0, E1 = 0, F1 = 0
c. A1 = 0, B1 = 0, C1 = 1, D1 = 0, E1 = 0, F1 = 1
d. A1 = 1, B1 = 1, C1 = 0, D1 = 0, E1 = 0, F1 = 0
Correct Response: (a)
Question: Your patient requires intermittent catheterization to relieve urinary retention and also experiences stress incontinence when sneezing. The best response for M1610, Urinary Incontinence or Urinary Catheter Presence would be:
a. 1 – Patient is incontinent and 2 – Patient requires a urinary catheter
b. 0 – No incontinence or catheter (includes anuria or ostomy for urinary drainage)
c. 1 – Patient is incontinent only
d. 2 – Patient requires a urinary catheter (i.e. external, indwelling, intermittent, suprapubic) only
Correct Response: (d)
Description: This Domain tests your mastery of OASIS item-specific guidance and scoring conventions for items collecting data on patient mood, and cognitive and behavioral status.
Sample Question for this Domain:
Question: After administering the first 2 sections of the BIMS ( C0100- Should the Brief Interview for Mental Status be Conducted and C0200- Repetition of Three Words), you are now administering the next section C0300-Temporal Orientation on Thursday, June 2, 2022. The patient provides the following responses to the orientation questions:
- Please tell me what year it is right now?- 2022
- What month are we in right now?- May
- What day of the week is today?- Saturday
With these responses, what is the correct coding for C0300. Temporal Orientation?
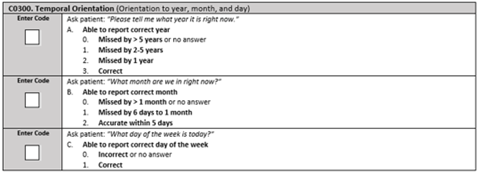
a. A. 3, B. 2, C. 1
b. A. 3, B. 2, C. 0
c. A. 3, B. 1, C. 0
d. A. 3, B. 1, C. 1
Correct response: (b)
Description: This Domain tests your mastery of OASIS item-specific guidance and scoring conventions for items collecting data on patient functional status using the OASIS M-function items.
Sample Question for this Domain:
Question: Your patient had abdominal surgery last week and now has an open wound which requires daily dressing changes. You are completing your comprehensive assessment and note that she is wearing a housedress with slippers and no socks. She tells you that she hasn’t tried to put on her regular clothes (which she describes as her underwear, pants, shoes and socks) because she is “afraid something will break” referencing her open wound if she bends too much. You ask her if she would try to dress while you are there with her and she demonstrates that she is too afraid and uncomfortable for the mobility required to dress her lower body. The patient usually wears pants, underwear, socks, and shoes with orthotic inserts.
The correct response for M1820, Ability to Dress Lower Body, would be:
a. 1 – Able to dress lower body without assistance if clothing and shoes are laid out or handed to the patient.
b. 2 – Someone must help the patient put on undergarments, slacks, socks or nylons and shoes.
c. 3 – Patient depends entirely upon another person to dress lower body
d. UK – Unknown
Correct Response: (c)
Description: This Domain tests your mastery of OASIS item-specific guidance and scoring conventions for items collecting data on patient medications, vaccinations and special treatments and procedures.
Sample Question for this Domain:
Question: On Tuesday, the Start of Care date, in order to complete the drug regimen review, the physical therapist provided the RN in the office with a list of all medications the patient was taking, the patient’s physical and cognitive status and details regarding the patient’s stated non-compliance with her prescribed oral antibiotic regimen which the therapist thought was a significant medication issue. The nurse finished the drug regimen review and called the report of the patient to the physician’s office. The physician’s office called the home health agency office nurse back on Wednesday with an appointment for the patient to be seen on Thursday. The agency nurse communicated the appointment to the patient immediately after speaking with the physician on Wednesday and also called the therapist to inform her of the physician’s response to the medication issue. The therapist used the information to complete the SOC assessment.
Based on this scenario, how would M2001 Drug Regimen Review and M2003 Medication Follow-up be answered on the Start of Care assessment?
a. M2001 = 0 – No. No issues found during review; M2003 = skipped
b. M2001 = 1 – Yes. Issues found during review; M2003 = 0 – No follow-up or completed interventions by midnight of the next calendar day.
c. M2001 = 1 – Yes. Issues found during review; M2003 = 1 – Yes – Follow-up and interventions completed by midnight of the next calendar day.
d. M2001= 9 – NA. Patient not taking any medications; M2003 = Skipped
Correct Response: (c)
Description: This Domain tests your mastery of OASIS item-specific guidance and scoring conventions for items collecting data on patient emergent care, inpatient admissions, discharges and transfer for health information.
Sample Questions for this Domain:
Question: Your patient had orthopedic surgery on her right hip on January 5th. After postoperative complications, she was discharged from the hospital to a rehabilitation facility on January 11th for therapy. She was discharged from the facility on January 19th. You are conducting the Start of Care assessment for an episode with a January 20th SOC date.
The correct response(s) to M1000, Inpatient Facility Discharges during the past 14 days, would be:
a. 3 – Short-stay acute hospital (IPPS)
b. 5 – Inpatient rehabilitation hospital or unit (IRF)
c. 3 – Short-stay acute hospital (IPPS) and 5–Inpatient rehabilitation hospital or unit (IRF)
d. NA – Patient was not discharged from an inpatient facility
Correct Response: (c)
Question: A record review indicated that Mrs. Black was admitted to the home health agency on August 30. Two weeks later she was seen in the ER for chest pain and released after treatment with a GI cocktail. Mrs. Black is in her second certification period and the nurse made a prn visit after receiving a call that the patient’s port-a-cath, used for chemotherapy, was oozing blood. After assessing the patient who also had complaints of weakness and nausea, the nurse placed a call to the physician who arranged for the patient to be directly admitted to a hospital bed where the patient remained as an inpatient for two days.
When completing the Transfer to Inpatient OASIS assessment, the correct response(s) for M2301, Emergent Care, would be:
a. 0 – No
b. 1 – Yes, used hospital emergency department WITHOUT hospital admission
c. 2 – Yes, used hospital emergency department WITH hospital admission
d. UK – Unknown
Correct Response: (b)
Description: This Domain tests your mastery of OASIS item-specific guidance and scoring conventions for items collecting data on patient self-care and mobility status and discharge goals using the OASIS GG-function items.
Sample Question for this Domain:
Question: Prior to her recent illness, Mrs. Cole walked around her home with a cane and supervision. During the SOC assessment, the physical therapist determines that it is unsafe for the patient to attempt ambulation and works with Mrs. Cole on lower extremity strengthening and balance activities. When completing the SOC assessment, GG0170I – Walk 10 feet would be:
a. 01. Dependent
b. 09. Not applicable
c. 10. Not attempted due to environmental limitations
d. 88. Not attempted due to medical conditions or safety concerns
Correct Response: (d)