
by Megan Bernier, MSPT RAC-CT COS-C
Ever wonder how your quality measures are impacted when a patient is transferred to an inpatient facility and a transfer OASIS is completed? To understand this, let’s first look at how OASIS-based measures are calculated.
Overview of Quality Measures
There are two types of OASIS-based quality measures in home health: process measures and outcome measures. Process measures evaluate the rate of home health agency use of specific evidenced-based care processes. Examples include the Timely Initiation of Care measure and Drug Regimen Review measure. Outcome measures indicate the change in patient status from one point in time to another point in time. Examples include Improvement in Ambulation/Locomotion and Stabilization in Grooming.
For quality measures to be calculated a patient must have a complete quality episode.
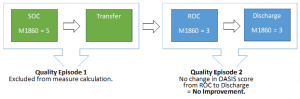
Quality episodes begin with either a Start of Care (SOC) or a Resumption of Care (ROC) and end with the next Transfer, Discharge, or Death at Home OASIS. Depending on the type of quality measure, the end of care OASIS (transfer, discharge, or death at home) can impact whether that quality episode is included in the measure calculation.
This is where Transfer OASIS (M0100 – Reason for Assessment, RFA-6 or RFA-7) can potentially have a huge impact on your quality measure calculation, specifically for the outcome measures.
When a Transfer OASIS is completed, that quality episode is excluded from most of the OASIS- based outcome measures. Since most outcome measures are a comparison of the patient’s status at the end of the quality episode compared to the beginning of the quality episode, there is no opportunity to capture any progress that patient made from the beginning of that quality episode when a patient is admitted for a qualifying inpatient stay as an in-person assessment does not occur with a transfer.
This initial quality episode (from SOC to transfer) is then excluded from the calculation of most OASIS-based outcome measures, like the Improvement in Ambulation/Locomotion measure and the Improvement in Bathing measure. When the patient returns to the agency and a ROC is completed, the ROC begins the next quality episode.
If the next end of care OASIS is a discharge OASIS, the outcome measures will be calculated by comparing the patient’s status on the Discharge OASIS compared to their status on the ROC OASIS. Essentially, any progress made from SOC to transfer is not included in the measure calculation.
For patients who are admitted to the hospital frequently while on home health services, this may impact progress on their outcome measures, in addition to the obvious negative impact on the claims-based measures like Discharge to Community measure and the Home Health Within Stay Potentially Preventable Hospitalization measure.
Example: How a Transfer Impacts Most Outcome Measures
Example 1: Improvement in Ambulation/Locomotion
In our first example, let’s look at the Improvement in Ambulation/Locomotion measure. To score favorably, the OASIS score at discharge for M1860 – Ambulation/Locomotion must be less than the score at SOC/ROC. In other words, the patient would have improved in ambulation/locomotion as indicated by the change (improvement) in OASIS responses.
In this example, at SOC M1860 – Ambulation/Locomotion is coded 5 – Chairfast, unable to ambulate and is unable to wheel self as the patient is unable to ambulate safely even with assistance. The patient received physical therapy (PT) and progressed to walking with assistance. Four weeks after the SOC, the patient was admitted to the hospital and a transfer OASIS was completed. At the ROC, M1860 – Ambulation/Locomotion was coded as 3 – Able to walk only with the supervision or assistance of another person at all times. The patient remained on services for three more weeks until they were discharged to an outpatient therapy program. At the time of discharge, they continued to require someone with them at all times to ambulate, therefore M1860 – Ambulation/Locomotion is coded as a 3 at discharge.
In this example, even though the patient made progress from SOC to Discharge, because the outcome measure calculation for Improvement in Ambulation compares the discharge M1860 score to the ROC M1860 score, for the purposes of the measure, the patient did not improve in the Improvement in Ambulation/Locomotion measure.
Example 2: Improvement in Bathing
Now, let’s look at an example with the Improvement in Bathing measure that is calculated using M1830 – Bathing. At SOC, for M1830 – Bathing the patient was coded 2 – Able to bathe in shower or tub with intermittent assistance of another person. The patient was very modest, highly motivated to become independent in bathing, but continued to require intermittent assistance due to weakness. They were then admitted to the hospital with pneumonia. Upon ROC, they were extremely weak and unsteady due to the episode of pneumonia.
M1830 – Bathing was coded 5 – Unable to use the shower or tub, but able to participate in bathing self in bed, at the sink, in bedside chair, or on commode, with the assistance or supervision of another person. Again, they were highly motivated to become independent, but the patient moved outside the agency’s service area to reside with their family two weeks after ROC. At discharge, M1830 – Bathing was coded 2 – Able to bathe in shower or tub with intermittent assistance of another person.
Example #2: Quality Episodes
In addition to OASIS accuracy, which is imperative for accurately reflecting patients in quality measure results, understanding quality measure calculations can be helpful in planning agency improvement strategies.
Additional information on quality measures, including which measures have exclusions related to a Transfer OASIS, can be found in the Home Health Quality Reporting Program Measure Calculations and Reporting User’s Manual Version 2.0 and the Home Health Outcome Measures Table.
___
by Megan Bernier, MSPT RAC-CT COS-C Why is item M1100 ...
by Marian Essey, RN, BSN, COS-C Soon after OASIS data ...
by Marian Essey, RN, BSN, COS-C With the October 2024 ...
by Lori Marmon PT, MBA, COS-C Beginning January 1, 2025, ...
by Kerry Termine, DPT, HCS-D, COS-C What are the Quality ...
by Lori Marmon PT, MBA, COS-C Home health providers are ...